Vaginal Hysterectomy for Prolapse
In this Health Topic
Prolapse is the loss of normal support of the vagina and/or uterus (womb). Prolapse of the uterus and/or vaginal walls is a common condition with up to 11% of women requiring surgery during their lifetime. Prolapse generally occurs due to damage to the supporting structures of the uterus or vagina. Weakening of the supports can occur during childbirth, following chronic heavy lifting or straining (e.g. with constipation), chronic cough, obesity, and as part of the aging process. In some cases, there may be a genetic weakness of the supportive tissues.
Prolapse of the uterus can cause an uncomfortable bulging sensation, a feeling of fullness, or pressure in the vagina. In more advanced prolapse the cervix can extend beyond the entrance to the vagina.
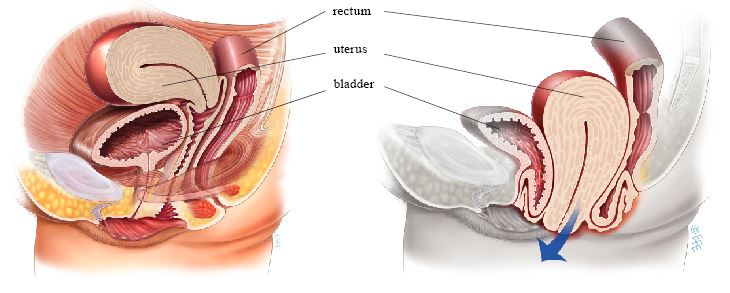
Normal uterus and vagina, no prolapse (left), and Prolapse of the uterus, bladder, and rectum (bowel) (right)
This is a procedure in which the uterus is surgically removed through the vagina. The operation is frequently combined with prolapse repairs of the bladder and/or bowel. There are no abdominal or laparoscopic incisions.
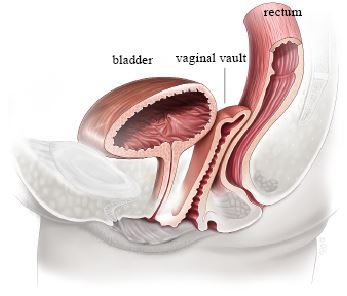
Appearance after hysterectomy
A vaginal hysterectomy offers many benefits over abdominal or laparoscopic procedures. It offers overall fewer complications, shorter healing time, less pain, less scarring, a lower chance of infection, less risk of hernias, and faster return to activities. Also, a prolapsed uterus is easier to access via the vagina.
The operation is performed in a hospital setting and can be performed under general or spinal anesthesia (with or without sedation). A cut is made around the cervix. The surgeon then carefully pushes the bowel and bladder away from the uterus. The blood vessels supplying the uterus and surrounding tissue are then clamped and secured. After confirming there is no bleeding, the surgeon removes the uterus and closes the top of the vagina, now known as the vaginal vault.
Many surgeons will choose to add additional support stitches to the vaginal vault at the time of surgery – either to the uterosacral ligaments that support the uterus (this is called a uterosacral ligament suspension) or to support structures on the side of the uterus (this is called a sacrospinous ligament suspension or ileococcygeus suspension). Leaflets are available on both of these procedures for more information. These additional stitches help to reduce the risk of the vaginal vault prolapsing in the future. Your doctor can explain what he/she plans to do. The ovaries can be removed during a vaginal hysterectomy if needed.
You will be asked about your general health, past medical history and any medication that you are taking. Any necessary tests (for example blood tests, ECG, chest X –ray) will be arranged. You will also receive information about your admission, hospital stay, operation and pre- as well as post-operative care. Mention to your doctor if you are on blood thinning agents such as aspirin, as these can lead to an increased risk of bleeding and bruising during and after surgery. Your doctor may ask you to stop the blood thinning medications 7 to 10 days prior to surgery. Some surgeons recommend bowel preparation prior to surgery.
When you wake up you will have a drip (IV) to give you fluids and you may have a catheter in your bladder. You may have a vaginal pack to reduce the chance of bleeding. Generally, the pack, catheter, and drip are removed in the first 24 to 48 hours after surgery. In most cases you will be able to eat and drink almost immediately after surgery. Pain and anti-nausea medication are given when needed, either intravenously, by intramuscular injection, or pill.
Keeping mobile after surgery is important to reduce complications such as clots in the legs and breathing problems, including pneumonia. Walking and light household duties are fine, however heavy lifting (more than 10kgs/25lbs) is not advisable in the first 6 weeks post-operatively. It is normal to feel tired following surgery so make sure you schedule rest times in the first few weeks after surgery.
You can expect to stay in the hospital 1-3 days. It is normal to get a creamy/brownish or bloody discharge for 4 – 6 weeks after surgery. This is due to the presence of stitches in the vagina. As the stitches absorb, the discharge will gradually reduce.
85% of women having a vaginal hysterectomy for uterine prolapse are cured permanently. About 15% of women develop a further prolapse of the vaginal vault months or years after their first surgery. These figures may vary depending on the severity of your original prolapse.
With any operation there is always a risk of complications:
- Anesthetic problems. With modern anesthetics and monitoring equipment complications due to anesthesia are very rare.
- Clots (embolism). After any pelvic surgery clots can form in the legs or lungs. This is a rare complication which is minimized by using support stockings and possibly blood thinning agents post-operatively (if indicated).
- Severe blood loss and hematoma. The risk of blood loss requiring blood transfusion is small (0-10%) and will in part vary on what other surgery you are having. About 10% of women develop a small collection of blood at the vaginal vault (a hematoma). This usually drains spontaneously after 7 to 10 days. Occasionally it will require surgical drainage.
- Infections. Although antibiotics are given just before surgery and all attempts are made to keep surgery sterile, there is a small chance of developing a vaginal or pelvic infection. This will usually present with an unpleasant smelling vaginal discharge and/or fever.
- Urinary tract infection. 6-20% of women having vaginal surgery develop a urinary tract infection. The risk is highest if you have had a catheter. Symptoms include burning and stinging when passing urine and frequency. If you think you have an infection after surgery contact your doctor.
- Injury to adjacent organs. Up to 2% of vaginal hysterectomies are complicated by either damage to the bladder, the ureters, or rectum. A very rare complication is the occurrence of a vaginal fistula.
- Urinary retention. In the first few days after surgery, difficulty passing urine can occur in up to 10-15% of cases. You may need to have a catheter for a few days after surgery until you are able to easily pass urine.
- Urinary incontinence. Prior to surgery, it is possible to have had urinary incontinence which was “occult” or hidden by the prolapse. During surgery, the urethra (the tube which empties the bladder) becomes unkinked or unobstructed, resulting in urinary incontinence becoming obvious post-operatively. This can occur in 40-45% of cases.
You should be able to drive and be fit enough for light activities such as short walks within a few weeks of surgery. You are advised to avoid heavy lifting and sport for at least 6 weeks to allow the wounds to heal. It is usually advisable to plan to take 2 to 6 weeks off work, depending on the type of surgery you have had and the type of work you do. Sexual activity can usually be safely resumed after 6 weeks.
