Colpocleisis
Colpocleisis (kaal·puh·klee·suhs) is a surgical procedure to correct advanced prolapse. Prolapse of the vagina or uterus is a common condition, with symptoms including a bulge or sensation of fullness in the vagina, or an external bulge outside of the vagina. It may cause a heavy or dragging sensation in the vagina or lower back and difficulties with passing urine or stool. 11-19% of women will undergo surgery for prolapse during their lifetime.
In this Health Topic
Colpocleisis (or vaginal closure) is an operation which corrects prolapse by irreversible sewing the front and back walls of the vagina together. This is often combined with perineorrhaphy where the weakened tissues of the perineum, situated between front and back passage is tightened. This prevents the vaginal walls from bulging either into, or outside of, the vagina and supports the uterus if it is present. Colpocleisis is only suitable for women who are not sexually active and do not intend to be sexually active at any point in the future, since the vagina will be closed off, not allowing vaginal intercourse. Nothing can exit the vagina (the bulge) or enter the vagina.
Colpocleisis can be carried out more quickly than other vaginal reconstructive procedures for prolapse, so it is particularly suitable for women with medical problems which may make them less suitable for longer and more complex operations. It is associated with high success rates (90-95%), and so may also be an option for non-sexually active women who have recurrent prolapse following previous surgeries. It can be carried out in women whether they still have their uterus or not.
If the uterus is still present, it can be removed (hysterectomy) at the time of colpocleisis. Le Fort Colpocleisis (partial colpocleisis) is the name of the vaginal closure surgery done when the uterus is still present and not removed. Small drainage tunnels are created during surgery to allow blood or mucus to drain from the uterus. It is very difficult to reach the uterus after healing from a Le Fort colpocleisis, thus, pre-operative testing is needed to make sure it is safe to leave the uterus. These tests include PAP smear, uterine biopsy or pelvic ultrasound.
Additional tests like bladder function test (urodynamics) or a kidney ultrasound may also organized by your specialist to assess bladder symptoms. If required, an operation for urinary leakage with physical exertion (stress urinary incontinence) can be performed along with colpocleisis.
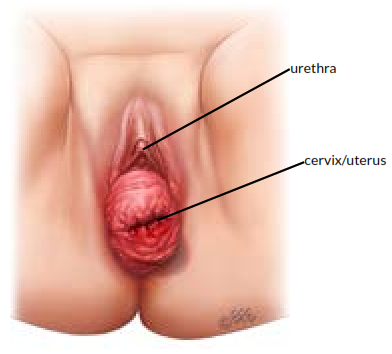
Front view of prolapse before surgery
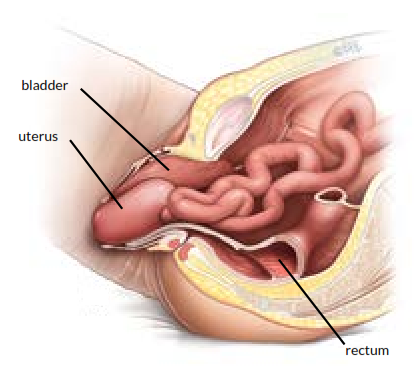
Side view of prolapse before surgery
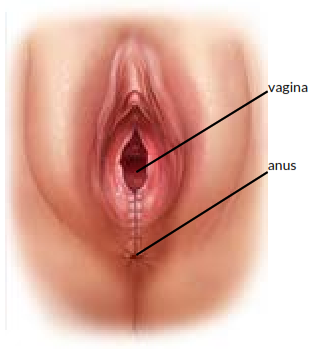
Appearance after colpocleisis surgery
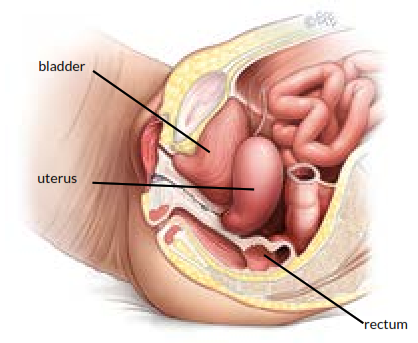
Side view of prolapse after colpocleisis surgery
You will be asked about your general health and medication that you are taking. Any necessary investigations (for example, blood tests, ECG, chest x-ray) will be organized. You will also receive information about your admission, hospital stay, operation, pre- and post-operative care.
Surgery requires either general or spinal anesthesia. When you wake up from the anesthetic you will have a drip (IV) to give you fluids and will have a catheter in your bladder. The catheter is generally removed 24-48 hours after the operation. You will be able to pass urine normally following a colpocleisis since the opening to the bladder is above the vaginal opening and thus is not affected by the procedure. If you have had a partial colpoclesis, a tubing (drain) may be placed along the channels created in the vagina at the time of surgery and removed in 12-24 hours. An overnight hospital stay is typical.
It is normal to have creamy white or yellow discharge for 4-6 weeks after surgery. The stitches in the vagina produce this discharge as they dissolve. As the stitches absorb, the discharge will gradually reduce. If the discharge has a bad smell, contact your doctor. You may see some blood-stained discharge immediately after surgery and after you walk or move about. This blood is usually quite minimal and old, brownish looking and is the result of the body breaking down blood trapped under the skin.
With any operation there is always a risk of complications. The following general complications can happen after any surgery:
- This is a common short-term problem, and your doctor may prescribe stool softeners or laxatives for this. Try to maintain a high fiber diet and drink plenty of fluids to help as well.
- Anesthetic problems. With modern anesthetics and monitoring equipment, complications due to anesthesia are very rare. Surgery can be performed using a spinal or general anesthetic. Your anesthesiologist will discuss this with you.
- Serious bleeding requiring blood transfusion is possible but uncommon for this surgery.
- Wound infection. Although antibiotics are often given just before surgery and all attempts are made to keep surgery sterile, there is a small chance of developing an infection in the vagina or pelvis. Symptoms include an unpleasant smelling vaginal discharge, fever, and worsening pain. If you develop these symptoms, contact your doctor.
- Bladder infections (cystitis). Cystitis occurs in about 6% of women after surgery. Symptoms include burning or stinging when passing urine, urinary urgency, and sometimes blood in the urine. If you develop these symptoms, contact your doctor. Cystitis is usually easily treated by a course of antibiotics.
- Blood clots in the legs/lungs (Deep Vein Thrombosis). Clots are more common in patients undergoing pelvic surgery. You will be given compression stockings to reduce the risk of this, and possibly also a course of injections.
Complications specific to colpocleisis:
- This is a collection of blood that can develop from the surfaces of the vaginal tissues that have been sewn together. This can cause pain and more bleeding than usual. Most hematomas will resolve by themselves but if that does not happen, your doctor may do a small operation to drain the clot. A hematoma can also become infected. This is treated with antibiotics.
- Rectal pressure. This decreases over time due to altered anatomy.
- Bladder and bowel injury. These are rare complications of vaginal prolapse surgery.
About 1 in 10 women do not feel satisfied with the outcomes of the surgery. This could be due to the recurrence of prolapse or because their initial symptoms have not improved after the operation.
About 1 in 5 women regret their decision later, as sexual intercourse is not possible after this operation. This could be avoided by considering other options of treating the prolapse and you should discuss this with your surgeon.
You should be able to drive when you can make an emergency stop and are fit enough for light activities such as short walks, typically within a few weeks of surgery. Remember to gradually build up your level of activity. You are advised to avoid heavy lifting and sport for at least 6 weeks to allow the wounds to heal. If you work, it is usually advisable to plan to take 4 to 6 weeks off. Your doctor can guide you as this will depend on your job type and the exact surgery you have had.
