Vaginal Pessary for Pelvic Organ Prolapse
In this Health Topic
Prolapse of the uterus (womb) and/or vaginal walls is a common condition affecting up to 50% of women. Up to 11% of women require surgery for prolapse during their lifetime. Prolapse generally occurs due to weakness of the supporting structures of the uterus or vagina. Weakening of the supports can occur during childbirth, as a result of chronic heavy lifting or straining e.g. with constipation, chronic cough, obesity and as part of the ageing process. In some cases, there may be a genetic weakness of the supportive tissues.
Prolapse of the uterus can cause an uncomfortable dragging sensation or feeling of fullness in the vagina, complaints of frequent urination, difficulty emptying the bladder/ and or bowel, and urinary tract infections. In more advanced cases, the prolapse can extend beyond the entrance of the vagina.
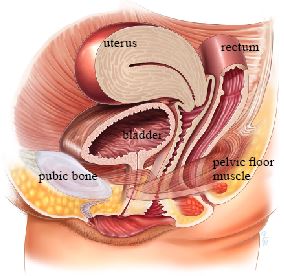
Normal anatomy, no prolapse
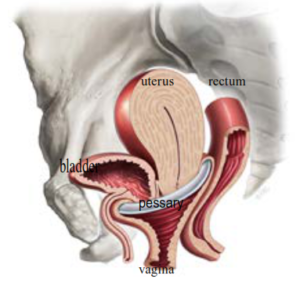
A vaginal pessary is a removable device that is placed in your vagina to support the weakened and prolapsed walls of the vagina or uterus. Different types of pessary are available: ring pessary with or without support, gellhorn pessary and a cube pessary are the most commonly used types of pessaries. Some pessaries such as ring pessaries can safely remain in the vagina for several months without removal. Others, such as the cube pessaries, must be removed and cleaned on a daily basis. Most pessaries are made from silicone, a soft non-absorbant material that poses no threat to your health. After a while the outer surface of the pessary can discolor. This is normal and does not mean that a new pessary has to be placed.

Types of Pessaries
Most pessaries are placed to improve symptoms of prolapse of the uterus and/or vaginal walls (see above). Sometimes your gynecologist will suggest a pessary to prevent or reduce urinary incontinence during exercise. In some cases you may want to use a pessary if you wish to avoid or delay surgery etc, if your family is not yet complete or if you have medical problems that will make surgery a risk.
Pessaries are fitted by first performing a vaginal examination to assess the type of prolapse. Your doctor will also measure your vagina to decide on the best type of pessary for your individual case. When the pessary is too small it may fall out, either on its own or when passing urine or during a bowel motion. A pessary that is too large may give pressure symptoms and feel too uncomfortable. Sometimes it can take a few attempts to find the most suitable size and type of pessary.
A minor prolapse may be treated with physiotherapy, while more severe prolapses may require an operation.
Once the pessary is inserted and placed appropriately in the vagina, it needs to be changed and checked at regular intervals. Practices between doctors vary but most will suggest that a pessary is cleaned or changed and the vagina checked every 3-6 months. Some women using ring pessaries are able to remove, clean, and replace the pessary themselves, otherwise this can be done at their doctor’s office. For some pessaries, such as the cube pessaries, daily removal is needed and they are therefore less suitable for longer term use. The gellhorn pessary is often used for more serious degrees of prolapse and this type of pessary usually requires removal by a doctor or nurse.
After menopause the vaginal skin thins due to a lack of estrogen. This may make the vagina dry and also more prone to ulceration when a pessary is in place. Your doctor may prescribe vaginal estrogen to improve the vaginal skin, making it healthier. Your doctor will discuss the possible indications for the use of estrogens and the consequences of use. For more information on vaginal estrogen treatment read our leaflet entitled Low-Dose Vaginal Estrogen Therapy.
The pessary should give women a solution without limitations to daily activity. For instance, you should be able to do sports, cycle and walk longer distances.
- Bleeding/ulceration to the vaginal wall. Depending on the type and size of pessary there is a chance that ulcerated areas may develop in the vagina. In this case you may experience a pinkish or bloody discharge. Ulcerated areas usually heal easily simply by removing the pessary for a short time. If you notice a bloody discharge, make an appointment with your doctor.
- Pain or discomfort. You should not be able to feel a pessary if it is correctly placed. If you experience significant pain or discomfort the pessary may be too large or small and require replacement with a different size. Talk to your doctor if this happens.
- Discharge. Most women experience a small amount of whitish discharge. With a ring in place this discharge may increase a little, but it should not be colored or unpleasant smelling. Both of these symptoms may indicate a vaginal infection and/or ulceration. Many doctors prescribe the use of vaginal estrogen cream to reduce the risk of ulceration. This can also result in an increased amount of creamy white discharge.
If you have a ring pessary it is possible to have intercourse with the ring in position. If you or your partner feel the ring with intercourse you can choose to remove the ring, replacing it again after intercourse. Other pessaries such as the doughnut, cube, or gellhorn pessaries largely fill the vagina and it is not possible to have sex while these pessaries are inserted. Make sure your doctor knows if you wish to be sexually active so that a suitable alternative pessary or other treatment can be planned.
